

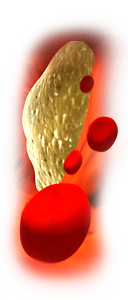
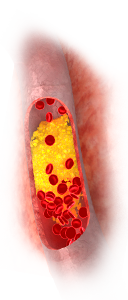
Atherosclerosis refers to the thickening of the walls of arteries caused by patchy deposits of fats and cholesterol usually covered by a fibrous (tough) cap. This causes the vessels to become narrow and the lining surface to become roughened. The surface of the fatty deposit may ulcerate (wear away) or rupture if a part of the fibrous cap breaks away. If this occurs, the blood can clot around the injured patch (a thrombus). This narrowing due to thrombosis can produce serious impairment of blood flow.
Atherosclerosis of the coronary arteries can cause angina and lead to deaths from heart attacks due to coronary thrombosis. When it affects the arteries supplying the brain it may cause impairment of mental function and thrombosis leading to a stroke. In the legs it may cause pains in the muscles on exercise, poor circulation to the skin and many other serious consequences.
There are many factors which are associated with coronary artery disease. We all know the risks of smoking, high blood pressure, high blood sugar, overweight due to overeating and not taking enough exercise. One key cardiovascular risk factor which has been shown to impact on longevity is the relationship between bad lipid levels and coronary artery disease. Bad lipid levels means one or more of increased blood levels of Low Density Lipoprotein (LDL or "bad") cholesterol, reduced levels of High Density Lipoprotein (HDL, or "good") cholesterol and raised blood fatty acids (triglyceride) levels. Other components of blood lipids have become the focus of clinicians in the management of atherosclerosis. For example, the European Atherosclerosis Society has recently published a consensus statement on Lipoprotein(a) which should now be considered a treatment target in intermediate and high risk patients independent of LDL and HDL cholesterol. Much of a person’s cholesterol level is determined by their genes. In families who suffer from high LDL cholesterol and/or triglyceride levels and in patients with disorders such as diabetes (in which these levels are increased) the incidence of coronary artery disease is markedly increased. There is some supportive evidence that in countries where diets are low in saturated fats, where genetic abnormalities of cholesterol are lower and where bad cholesterol and triglyceride levels are lower , the incidence of coronary artery disease is reduced.
After a person’s genes, the most important factors affecting blood cholesterol levels are diet and lifestyle. Diet changes can alter ratios of good and bad cholesterol mainly because of changes in the type and ratio of different fats in the diet. The ratio of unsaturated fatty acids (in vegetable and fish oils) to saturated fatty acids (in animal fats and dairy produce) is a key factor. Therefore, a reduction in the overall consumption of fats, a decrease in animal fats, and a proportional increase in vegetable and fish-derived fats over animal fats may help to reduce blood cholesterol and triglyceride levels.
Lifestyle changes apart from the diet can also help improve the blood lipid profile. For example, more regular exercise, reduced smoking and reduced alcohol intake all can increase HDL or "good cholesterol" levels, reduce triglycerides and reduce LDL.
In people who do not achieve ideal cholesterol levels (see Table 1), the good news is that there is now a considerable amount of evidence that effective lowering of LDL cholesterol and triglycerides with medicines can reduce deposits in arteries and reduce the risk of coronary artery disease. This evidence is most convincing where medicines called "statins" have been used. A 10% reduction in plasma total is followed by a 25% reduction in the incidence of coronary artery disease after 5 years. A reduction in LDL cholesterol of 1mmol/L (40 mg/dL) is associated with a 20% reduction in coronary heart disease events. However, even when a person is prescribed medicine for modifying cholesterol levels, healthcare professionals will advise that diet and lifestyle improvements should continue.
Another important point to note is that while doctors will usually advise diet and lifestyle changes first, before resorting to medication, in some people cardiovascular risk factors tend to "accumulate". For example, when people have blood cholesterol problems, they often have other cardiovascular risk factors such as high blood pressure, overweight and high blood sugar levels. In people with several cardiovascular risk factors, doctors may be inclined to prescribe medication earlier.
Also, there is now evidence that some medicines that affect cholesterol have other benefits. For example, it is known that inflammation in the body can accelerate the rupture of the fibrous cap on fatty deposits in the arteries. Some of the medicines used to improve blood cholesterol levels, such as statins and nicotinic acid, also reduce proteins associated with inflammation in the blood. Exciting new studies have shown that statins can reduce mortality in people with normal cholesterol but with high levels of a marker inflammation protein called C-Reactive Protein (CRP).
Plasma Lipid Type |
Treatment Goal |
Total Plasma Cholesterol |
< 5 mmol/L (190 mg/dL) |
LDL Cholesterol |
< 3.0 mmol/L (115 mg/dL) |
Lipoprotein (a) |
< 50 mg/dL in intermediate or high risk patients |
HDL Cholesterol |
No specific treatment goal, but levels < 1.0 mmol/L (40 mg/dL) in men and <1.2 mmol/L (45 mg/dL) in women serve as indicators of increased risk |
Triglycerides |
No specific treatment goal, but levels > 1.7 mmol/L (150 mg/dL) serve as indicators of increased risk |
Table 1. Treatment targets for different plasma lipid components (adapted from European Society of Cardiology 2007 Guidelines on cardiovascular prevention in clinical practice.)
The statin group of drugs include:
They block the production of cholesterol in the liver and reduce blood levels of cholesterol and also triglycerides. Treatment with statins has been shown to reduce heart attacks and death from heart disease. They are the drugs of choice in patients with a high risk of coronary heart disease because they have been shown to reduce mortality most convincingly in a number of large studies. Statins are mainly used to reduce LDL, but they also have a modest effect on HDL and triglycerides. Recently, rosuvastatin has also been shown to reduce mortality in patients with normal cholesterol levels and high levels of an inflammatory protein, CRP, in their blood.
Cholesterol synthesis in the liver reaches a peak at night. If statins are long acting (atorvastatin and rosuvastatin) they can be taken at any time of the day and still remain effective. Other statins should ideally be taken at night time to be at their most effective.
All statins can cause abnormalities of muscle proteins and any "myopathy" or muscle pain should be immediately investigated by the patient’s doctor, who may change to another statin or discontinue the medicine. Also, the patient should be screened for rare but serious abnormalities in liver function.
Nicotinic acid (Niaspan, in Tredaptive) in high doses is the most effective agent on the market for boosting HDL or "good" cholesterol. It also reduces LDL cholesterol, Lipoprotein(a) and triglycerides. New European Atheroscleosis Society consensus guidelines confirm that nicotinic acid at a dose of 1-3g per day is the agent of choice in reduction of lipoprotein(a) levels.
However, in the past it has been of limited use because of its adverse effects. Patients experience uncomfortable flushing, headache and itching. This usually clears after a few weeks in most patients and may also be improved by slowly increasing the dose over several months, by taking the medicine at bedtime and also by taking aspirin half an hour before the nicotinic acid. The most commonly prescribed form of nicotinic acid is a modified release oral tablet which causes reduced flushing (Niaspan). In Europe but not the US, a new type of modified release nicotinic acid combined with an "anti-flushing" agent has been licenced (Tredaptive). Neither of these methods can completely stop the flushing problems with nicotinic acid and they also can cause a small but significant rise over time in plasma glucose levels. Very large dose of nicotinic acid may also cause liver damage and jaundice in a small number of patients over time, and close monitoring of liver function is required. Acipimox (Olbetam) is structurally related to nicotinic acid, has similar benefits and less side-effects, but is less potent.
Ezetimibe (Ezetrol) is a relatively new type of LDL cholesterol-lowering drug which works by decreasing absorption of cholesterol in the intestine. It may be used alone, but is often used as an addition to statin therapy when LDL levels remain persistently high. It is often well tolerated, with headache and/or diarrhoea being the most common adverse effects. However, good information that these agents can improve mortality is not yet available and so its use in practice is limited to occasions when other cholesterol modifying therapy does not work or is not tolerated by patients.
The fibrate group of drugs fenofibrate (Lipantil) and gemfibrozil (Lopid). These drugs are effective in lowering cholesterol and triglycerides although their mode of action is not fully understood. Long-term use of these drugs may damage the muscles, particularly in patients with impaired kidney function.
Bile acid sequestrants include colestyramine (Questran) which reduces blood cholesterol levels. It works in the intestine by exchanging chloride ions for bile salts (which are formed in part from cholesterol) which the drug binds into an insoluble complex that is excreted in the faeces, so preventing the reabsorption of bile salts and cholesterol. This causes further conversion of cholesterol to bile salts, which eventually may lead to a reduction in blood cholesterol. It may also interfere with the absorption of other drugs (chlorothiazide, phenobarbitone, tetracyclines, thyroid hormones and many others). High doses interfere with the absorption of fat and fat-soluble vitamins, such as vitamins A and D; therefore, no other drug should be taken within one hour of a dose of colestyramine. Extra vitamin A and D should be taken, of a type that can be mixed with water; patients on prolonged treatment should also take vitamin K.
Fish oils (in Maxepa, Omacor) are polyunsaturated fatty acids, rich in omega 3 and 6 triglycerides, which lower cholesterol and triglyceride levels. Although they are available in capsules, they can cause uncomfortable "fish burp". Nonetheless, they have been shown in some studies to provide modest but significant improvements in some patients.
Ispaghula husk (Fybogel Citrus) contains both insoluble fibre and soluble fibre. The latter has been shown to reduce blood cholesterol levels by reducing the absorption of cholesterol and fatty acids from the intestine, by binding bile acids resulting in their increased excretion. As a consequence, the liver has to use more cholesterol to manufacture bile salts, leading to a fall in the blood cholesterol level. However, plasma triglyceride levels remain unchanged.
As outlined in Table 1, the desirable level of total cholesterol is 5.0 mmol/L or below, together with LDL cholesterol levels of 3.0 mmol/L or less. HDL levels are naturally higher in women than in men and should ideally be above 1.0 mmol/L for men and above 1.2 mmol/L in women. Triglyceride levels should ideally be below 1.7 mmol/L.
As a secondary priority after LDL cholesterol reduction in "intermediate risk" patients (i.e. those with familial hypercholesterolaemia, a family history of premature cardiovascular disease and a 3% 10-year risk of fatal cardiovascular disease according to European guidelines) plasma lipoprotein(a) levels should be treated to ensure they are below 50 mg/dL.
In "high risk" patients, for example those with established cardiovascular disease and/or diabetes, the level of plasma total cholesterol should be 4.5 mmol/L or below and even lower (< 4.0 mmol/L) if feasible. LDL cholesterol levels in high risk patients should be 2.5 mmol/L or less and even lower (< 2.0 mmol/L) if feasible. In these patients lipoprotein(a) levels should be below 50 mg/dL.
As discussed above, abnormal levels of cholesterol and/or triglycerides present a high risk if they are associated with other risk factors such as smoking, raised blood pressure, diseases of the circulation, diabetes, severe obesity and/or a family history of raised blood fats and/or coronary artery disease. In these cases, doctors will often use high doses of statins and combination therapies.
Treatment should start with, and always involve, a healthy diet and regular exercise where possible. Improved lifestyle, including stopping smoking and reduced alcohol intake, is always advised even when medicines are used to improve blood cholesterol levels. Finally, reduction in other modifiable risk factors if elevated, such as blood pressure and blood sugar, should always be part of the approach to the management of abnormal cholesterol levels.
Currently, therapy for lipid modification for atherosclerosis treatment and prevention focuses on lowering LDL cholesterol. However, despite the notable progress in reducing cardiovascular risk with "statins", cardiovascular disease continues to be the leading cause of death and disease worldwide. As a result, novel strategies to address this residual risk have been sought. Combination therapy is now being advocated for many patients. In these cases the careful selection of correct combinations and ongoing patient monitoring is essential. Also, abnormal HDL cholesterol still remains a significant cardiovascular risk factor. New medicines in the future will focus on improving HDL levels in a complementary way to statins.
Prof. Peter Weedle is a community pharmacist and adjunct Professor of Clinical Practice at the School of Pharmacy, University College Cork. Peter has a wide range of interests in the area of pharmacy but in particular, medicine use by the elderly, drug interactions, legal and ethical matters. He is co-author of two books: Pharmacy and Medicines Law in Ireland and Medicines: A guide for everybody. This series is based on Medicines: A guide for everybody which was originally published by Penguin, London. Peter can be contacted at: pweedle@icloud.com
Dr. Mark Ledwidge is a pharmacist with a research and teaching interest in Cardiovascular Disease. In particular, his interests include medication adherence in chronic illness, telemedicine and cardiovascular therapeutics. He is Director of Heart Failure Research in St Vincent’s University Hospital and Adjunct Senior Lecturer in the School of Medicine in University College, Dublin.
Dr. Andrew Fisher is a community pharmacist in Cork City, with an extensive research background in neurological disorder and disease. His particular areas of interest include the pathophysiology and treatment of basal ganglia disorders and epilepsy. Andrew has a wide range of interests within the field of pharmacy including patient compliance, pharmacovigilance and therapeutic drug monitoring.
Mr. Nigel Moloney is a Superintendent Pharmacist in Cork city. Nigel comes from a UK Hospital Pharmacy background and his primary interests are in Acute Medicine, Psychiatry and Risk Management. Nigel has published articles in the scientific press on Risk Management Quantification and Communication between Primary and Secondary Care.
Dr. John McAninly is a community pharmacist in Mallow, Co. Cork who worked in hospital and community pharmacy in the UK, before moving to Ireland. As a former teacher he has a special interest in pharmacy education.

We accept responsibility for the text and any views expressed therein. While every effort has been made to ensure accuracy, we accept no liability for errors or omissions. If you have concerns about the medicines you are taking please speak directly to your pharmacist or your physician.

We at Drug Adviser respect your right to privacy and have created this statement in order to comply with our obligations under the Data Protection Acts. The purpose of this website Privacy Statement is to outline how we deal with any personal data you provide to us while visiting this website. By visiting this app, you are accepting the terms of this Privacy Statement.
Personal Data
We will process any Personal Data you provide to us for the following purposes:
a) to provide you with the information requested;
b) to contact you if required in connection with your enquiry or to respond to any communications you might send to us;
c) If you complete one of our contact forms, we will use that information to contact you. After that initial contact if you wish not to be contacted again we will respect that and delete your contact information.
d) If you would like us at anytime to delete your information we will gladly do so. Simply email us with the request and we will comply.
Any contact information that you provide through our system will NOT be sold/rented/leased to any third party for the purpose of selling or marketing to you and will be kept private.